35 year old man with DCMP
35 year old man working as a food caterer presented to our OPD with the chief complains of
Dyspnea at rest since 5 days
Cough with expectoration since 5 days
Bilateral pedal edema since 4 days
Abdominal distension since 3 days
He was a regular alcoholic since the past 10 years and an occasional smoker. He apparently was completely alright until one morning in November 2019 when he had high fever with chills and visited a local hospital where he got admitted, he says the fever was intermittent and more at nights and was often followed by sweating and was diagnosed with malaria for which he received treatment.
In Dec 2019, the following month, he says he started feeling breathless while climbing up the stairs which progressed over the next 5 days to such an extent that he even felt dyspneic even at rest and had dry cough on and off. He says that his dyspnea and cough aggravated on laying in bed. He gradually developed bilateral pedal edema followed by abdominal distension over the next few days which alarmed him and he decided to pay a visit to a doctor. He visited a local hospital and was put on some medications ( no documentation ) which patient couldn't recall of. Since it did not improve his symptoms he visited our hospital in January 2020.
He however gave no complaints of palpitations, nausea, vomiting, profuse sweating.
He also gave no complaints of reduced urine output, hematuria, forthy urine.
No complaints of burning micturation, diarrhea, vomiting, pain abdomen.
PAST HISTORY:
Since the past 10 years he has been consuming around 180 ml of whiskey everyday. He also tells that he would occasionally smoke cigarette once in a while along with his friends. In those 10 years he never paid a visit to his hometown due to financial issues and decided not to get married anytime soon as he wanted to settle the financial issues his family was facing.
Not a known case of Diabetes, Hypertension, Also no history of CAD, CVA, Bronchial Asthma, Pulmonary Koch's.
On presentation to our hospital:
He was obese with central obesity
His pulse rate was 100 bpm
Blood pressure - 110/70mmhg
RR - 21 cpm
Spo2 - 98% on Room Air
Temp - 98.6 %
GRBS - 151 mg/dl
GENERAL EXAMINATION:
He weighed 98 kgs and his abdominal girth measured 100 cm
He had no pallor, icterus, clubbing, cyanosis, lymphadenopathy
He had bilateral pitting type of pedal edema present upto his knees
JVP was raised
SYSTEMIC EXAMINATION:
CARDIOVASCULAR:
Inspection:
Shape of the chest - Ellipsoid
No dilated veins, scars, sinuses
No cutaneous lesions
No breast abnormalities
Palpation:
Apex beat palpated in 6th ICS 1 cm lateral to MCL
No palpable pulsations in aortic or pulmonary area or tricuspid area
No palpable pulsation
No palpable epigastric pulsations
No palpable pulsations in sternoclavicular area
Auscultation:
Muffled S1,S2 +
RESPIRATORY SYSTEM EXAMINATION:
Inspiratory crepitations in Bilateral in IAA, ISA
PER ABDOMEN:
soft
Non tender
No organomegaly
Bowel sounds +
CENTRAL NERVOUS SYSTEM EXAMINATION:
Normal
PROVISIONAL DIAGNOSIS:
HEART FAILURE SECONDARY TO
? VIRAL MYOCARDITIS
? ALCOHOLIC
REPORTS:
ECG:
His blood picture, renal and liver parameters were in within the normal range.
On routine investigations his HbA1c was found to be 8.4 %.
His Ultrasonography of abdomen revealed Grade 1 fatty liver ( probably secondary to his alcohol intake), mild ascites, Right moderate pleural effusion.
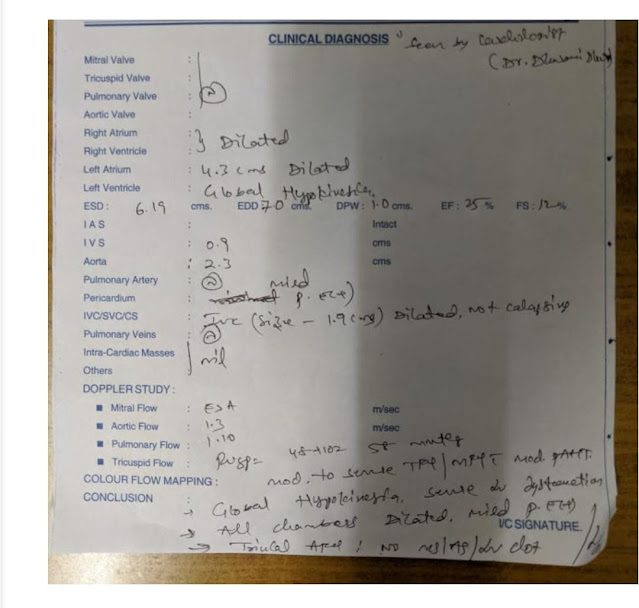
2DEcho was done which revealed that all the 4 chambers to be dilated with an ejection fraction of 27, global hypokinesia, severe MR, trivial AR, severe LV dysfunction with mild PAH, dilated IVC (2.3cm)
A diagnosis of HEART FAILURE WITH REDUCED EJECTION FRACTION - 27%
DENOVO DETECTED TYPE 2 DIABETES MELLITUS
TREAMENT ADVISED:
he was started on
1. Tab Lasix 80mg in the morning, 40mg in the afternoon and evening
2. Tab Isosorbide mononitrate 10mg twice a day
3. Tab Hydralazine 25mg
4. Tab Telma 40mg
5.Tab Metformin 500mg once a day
and was advised for fluid of less than 1 litre and salt restriction of less than 2grams/day
He was advised for a coronary angiogram for which he visited Hyderabad. CAG was performed on 24th of January 2020 which turned out to be normal and he was started on Tab Vymada 50mg and Tab Met XL 12.5mg
( Sacubitril 26 mg and Valsartan 24 mg) along with Tab Ecosprin AV (75/20)
On regular at home monitoring of blood glucose levels which were within the normal range, he stopped taking Tab Metformin.
On 14th March 2020 he paid a visit to our hospital with the similar complains and a review scan of 2DEcho was done which revealed end point septal separation distance to be increased and Tab Vymada was increased to 100mg.
On July 28th, 2020 he presented to our OPD with the complains of Dyspnea at rest since 5 days which apparently aggravates when the patient is in supine posture and he also complains of occasional cough with scanty mucoid, non blood tinged sputum especially while he is asleep. He says he developed bilateral pedal edema extending upto his knee over the past 4 days followed by abdominal distension.
Patient appears to have gained weight with abdominal girth measuring 116cm and he weighed 101 kg
He weighs 93 kgs now
He appeared to be in respiratory distress with a respiratory rate of 28 cycles per minute and his saturation was at 98 % on room air.
His heart was beating at 120 bpm with a blood pressure of 100/70mmhg.
He was afebrile.
He had Icterus
His JVP was raised
CVS:
On palpation:His apex beat was in 6th intercostal space, 1cm lateral to midclavicular line.
On auscultation, S1 S2 +
His lungs were clear on auscultation
His abdomen was soft to palpate and bowel sounds were heard.
CNS: Normal
Hemogram:
Hb - 13 g/dl
TLC - 7000 cells/cumm
Platelet count - 2.28 L/cumm
Complete Urine Examination:
showed no albumin, sugars, RBCs
2-4 Pus & epithelial cells
Renal Function Test :
Urea - 53 mg/dl
Creatinine - 1.4 mg/dl
Uric Acid - 9 mg/dl
Calcium - 9.6 mg/dl
Phosphorus - 3.3 mg/dl
Sodium - 133 mEq/L
Potassium - 4 mEq/L
Chloride - 98 mEq/L
Liver Function Test:
Total Bilirubin - 4.60 mg/dl
Direct Bilirubin - 2.42 mg/dl
AST - 56 IU/L
ALT - 44 IU/L
ALP - 129 IU/L
Total Proteins - 6.2 gm/dl
Albumin - 3.9 gm/dl
His 2Decho showed dilated chambers with global hypokinesia, ejection fraction of 26 %, severe MR, mild TR, Trivial AR, mild pericardial effusion, mild PAH and IVC measuring 1.7 cms.
The Patient is currently on fluid and salt restriction
Along with INJ LASIX 40MG TID
TAB VYMADA 100 MG BD
TAB VALSARTAN 80MG OD
TAB MET XL 12.5MG OD
TAB DYTOR PLUS 10/25 OD













Comments
Post a Comment